Oral and Jaw Surgery
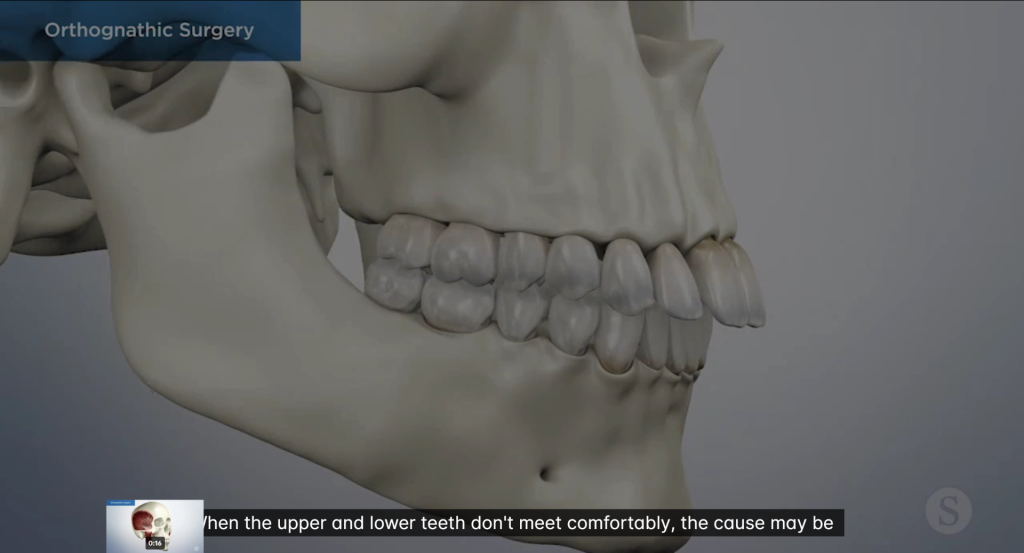
Orthognathic Surgery
Advancements in dentistry have led to the development of various non-invasive treatment procedures. But this has not eliminated the need for oral surgeries. One of the common dental surgeries that, according to research, as many as about 15% of people with tooth and jaw abnormalities may need is called orthognathic surgery.
Wondering what that complex-sounding surgery involves and who needs it? Keep reading as we discuss all the essential details about orthognathic surgery.
What is Orthognathic Surgery?
Orthognathic surgery is the professional name for corrective jaw surgery. Simply defined, the procedure involves realigning the jawbones. It could be done to just one jaw (upper or lower) or both.
The orthognathic surgery can be used to shorten or lengthen the jaw and move it in or out or up and down. The primary goal of this reconstructive jaw surgery is to fix irregularities of the jawbones to improve their function and bite, but many people also notice an improvement in their speech and appearance after it.
Most often than not, orthognathic surgery involves a series of steps over time. These may include certain orthodontic treatments before the surgery to prepare your mouth and teeth, the actual surgery to correct issues, recovery and follow-up orthodontic treatments and/or maintenance procedures that could continue for up to a year. The whole surgical procedure can take up to two to three years.
Who Needs Orthognathic Surgery?
Orthognathic surgery is used for people with jawbone irregularities that cannot be fixed by non-invasive orthodontic procedures alone. These typically include severe misalignments of the teeth (malocclusion), misaligned jaw and improper bite.
Here are some of the jaw abnormalities that may require orthognathic surgery:
- Asymmetrical jaws
- Severe underbite
- Severe overbite
- Open bite
- Crossbite
- Cleft lip and palate
- Pierre Robin sequence – a condition characterized by a small or underdeveloped lower jaw that makes it difficult to eat and/or breathe.
What are the Benefits of Orthognathic Surgery?
Orthognathic surgery may be a long and complex procedure, but it can greatly relieve those suffering from jaw abnormalities. Here are some of the most well-known benefits of corrective jaw surgery:
- Improved bite and chewing (functioning of teeth)
- It corrects problems with swallowing
- Correct speech impairment issues
- Fix jaw misalignment issues and makes sure your jaw closes the right way
- Fix facial imbalances due to improper aligning of jawbones. These may include crossbites, underbites, overbites, and small chins.
- Relief from jaw pain
- Improved lip closure, more comfortably.
- Fix various oral congenital disabilities (birth defects0 or issues resulting from facial injuries
- Orthognathic surgery also helps provide relief from obstructive sleep apnea.
Who Performs Orthognathic Surgery?
Orthognathic surgery is a complex, multi-step procedure that requires the involvement of multiple dental care professionals at different stages. But, your surgeon and the orthodontist have the most important jobs.
At Ortodontist, we have some of Turkey’s most experienced orthodontists and oral surgeons on board. Get in touch with us for a detailed oral examination if you experience any jaw alignment issues and determine if you’re a candidate for orthognathic surgery.
TOOTH EXTRACTION
Dental issues can be a source of dread for us. It’s no surprise that toothache may be excruciating and can hinder your ability to work.
If your tooth has suffered severe damage that can not be repaired, extraction may be required. If you have severe tooth cavities, a fractured tooth, an impacted tooth, crowded teeth or severe gum disease your dentist may extract your tooth.
Although it is generally imperative to protect your teeth, there are some cases where extractions are necessary. The causes include trauma, infection, and dental crowding.
The best course of action may be to pull a tooth if it cannot be restored with a crown or filling. Periodontal disease-related teeth that lack sufficient bone support and abscessed (infected) teeth that cannot be saved by root canal therapy may require extraction.
An orthodontist may advise one or more extractions before braces if your teeth are crowded. Like the impacted teeth, wisdom teeth are commonly removed because they may not have enough room to emerge into the mouth or are entirely compromised.
Simple Extraction
These tooth extractions are often carried out on teeth exposed in the jaw and are typically done with a local anesthetic is a simple extraction.
Surgical Extraction
When a tooth is difficult to reach, surgical extraction methods are used. It happens when a tooth has not completely developed or has been damaged beneath the gumline.
The dentist may make an incision to expose the soft tissues around the tooth during this operation. The tooth may sometimes be divided into many pieces to make removal more manageable. General anesthesia is typically used to do surgical extractions.
It is best to consult your dentist to decide which procedure should be opted for in your case.
Your dentist can typically establish whether you require a surgical or simple extraction by performing an x-ray and looking at your tooth. For instance, the dentist might need to perform a more involved surgical procedure if a tooth falls out between the course.
Surgical extractions are also performed for the following reasons:
- When the removal of wisdom teeth requires cutting the tissue and bone if they are compromised
- When pulling out damaged teeth
- When removing root tips or long-curved roots from teeth
- When a molar or tooth is fractured at the gum line
Several factors should be anticipated when having dental extractions. Removals are now easier than ever, thanks to modern technology. Some sedative alternatives are available if you prefer not to be conscious throughout the treatments.
Depending on the circumstances, many tooth extraction procedures can be painless. The discomfort should not be worse than getting a tooth filled. The use of essential medications, such as mefenamic acid and acetaminophen, can provide relief.
It will not take more than a few weeks for the wound after a tooth extraction to recuperate. Most of the time, there are no complications; only infections can cause problems.
The post-extraction pain subsides within a day or two in most cases.
A heavy oral activity like chewing and ice-crushing should be avoided at that duration. Oral rinses and cold packs are effective pain relievers at home. Food consumption needs to be restricted.
Complete tooth extraction recovery takes at least a month and in rare circumstances about two months. Your healthcare practitioner should perhaps offer you a recovery plan.
Wisdom Tooth Extraction
Do Wisdom Teeth Really Have To Come Out?
Wisdom teeth in most people fail to erupt either partially or entirely. In America, approximately 70% of young adults would probably have one wisdom tooth that has not yet erupted. For those with smaller space in the back of their jaw, wisdom tooth eruption is often painful.
The average person has four wisdom teeth, with one in each corner. In the teenage years or early twenties, wisdom teeth often erupt through the gums. There may not always be enough space in the jaw for the wisdom teeth to erupt fully by this time, while the other 28 permanent teeth are typically in position.
Most often, dentists and oral surgeons only advise getting wisdom teeth extracted if they are already causing difficulties or are likely to do so in the long run. Even now, there are no benefits to getting rid of your final set of molars if they aren’t bothering you. Furthermore, wisdom teeth removal is uncomfortable and might have some untoward side effects.
So before deciding if you want to get rid of your pearls of wisdom, here are some signs of problematic wisdom teeth, surgical options and post-surgery care.
Wisdom teeth can cause complications if there isn’t sufficient space for eruption or if they develop in the wrong position. If your dentist describes your wisdom teeth as being impacted, it indicates that they are stuck either in your jaw or the gums.
Your dentist will keep an eye on your mouth when your wisdom teeth erupt to look for the following symptoms:
Ø Food can become lodged around the wisdoms that are not properly positioned. This provides a habitat for bacteria that cause cavities.
Ø Wisdom teeth that have not fully developed, making it harder to floss around that area.
Ø Partially erupted wisdom teeth might provide a pathway for germs to penetrate the gums and cause an infection. Also, your jaw may become sore, swollen and stiff.
Ø Wisdom teeth might crowd or harm other teeth if they do not have enough room to erupt.
Ø An impacted wisdom tooth might develop a cyst on or close to the tooth. This could harm surrounding the tooth’s roots or the bones supporting your teeth.
Consult your dentist to learn more about the position of your wisdom teeth. To examine the development and placement of your wisdom teeth, they could do an X-ray on you from time to time. Your dentist may potentially refer you to an oral surgeon for additional assessment.
Before any possible complications, your oral surgeon could advise removing your wisdom teeth. Earlier detection and extractions can save you from more difficulties in the future. Wisdom tooth extraction is relatively easier in younger adults since the wisdom teeth’s roots are still developing and the bone is soft. Healing and recovery typically take longer in elderly adults.
Consult your dentist to learn more about the position of your wisdom teeth. To examine the development and placement of your wisdom teeth, they could do an X-ray on you from time to time. Your dentist may potentially refer you to an oral surgeon for additional assessment.
Before any possible complications, your oral surgeon could advise removing your wisdom teeth. Earlier detection and extractions can save you from more difficulties in the future. Wisdom tooth extraction is relatively easier in younger adults since the wisdom teeth’s roots are still developing and the bone is soft. Healing and recovery typically take longer in elderly adults.
Only a small percentage of adults over 30 have difficulties with their wisdom teeth. Wisdom can be a problem for younger adults between the ages of 15 to 25. A wisdom tooth extraction, however, could be necessary at any age.
These signs indicate you should get your wisdom teeth removed:
The Back of Your Mouth Is Sensitive and Painful.
The earliest and most evident indicator when you need your wisdoms pulled out is when you start to feel them. If you begin to feel discomfort, sensitivity or a slight throbbing feeling when eating, cleaning your teeth or even while doing nothing, it’s time to visit your dentist to examine it.
Inflamed Gums.
You may experience gum tenderness when your wisdom teeth start to erupt. It will manifest as reddish, somewhat swollen regions mainly along the gum line that hurt to the touch and may even make it difficult to brush your teeth properly.
Cysts in Your Mouth.
If you have been neglecting the pain and inflammation from the erupting of a wisdom tooth, there are chances that you may develop a cyst around the tooth. Cysts are sacs filled with fluid that may end up affecting and harming the roots of nearby teeth.
Jaw Stiffness and Discomfort.
Since wisdom teeth have the potential to start shifting the teeth and jawline, stiffness and discomfort can also develop around the jaw. This might also be indicated by having difficulty moving your jaw and opening your mouth.
Sinus Problems.
Most people don’t realize that any complications with oral health can affect the sinuses, and complications with wisdom can be one of them. When your sinuses are congested, painful or under pressure, this may indicate that you should have your teeth extracted.
Unpleasant Taste and Bad Breath.
The sensitive gum tissue surrounding impacted or misaligned wisdom teeth are often not properly cleaned, resulting in lodged food particles and plaque deposition that over time can cause an infection. Because of the resultant germs, you may constantly taste something nasty in your mouth and have awful breath.
Caries and Tooth Decay.
Your wisdom teeth’s positioning might significantly affect how well you can clean areas where germs might congregate. Bacteria that thrive in inflamed gum pockets can encourage the formation of cavities and ultimately an infection.
Misalignment of Adjacent Teeth.
The third set of molar teeth usually cannot fit in our jaws because they are too small. They so develop sideways and snag on neighboring teeth. Other teeth may displace if the wisdom teeth erupt unevenly or crookedly.
Your wisdom teeth’s position and developmental stage will affect how easily your oral surgeon can remove them. You can better understand what to anticipate from your pre-extraction evaluation from your dental health care professional.
Before Surgery
The oral surgeon will meet with you to discuss the procedure. During your consultation, be sure to:
Ø Discuss any health issues you may have.
Ø List any medications you regularly take.
Ø Request any information you want on the procedure.
Ø Understand the type of anesthetic you will get. During your procedure, you may be awake or unconscious.
Ø Make arrangements for a period off from school or work so that you can recover at home following surgery.
During Surgery
The surgical extraction will take no more than 45 minutes.
One of these forms of anesthetic will be administered to you so that you will not experience any discomfort during surgery:
Ø Local anesthetics like lidocaine, mepivacaine, or novocaine will be injected into your mouth to numb it. Laughing gas, commonly known as nitrous oxide, can be used during surgery to help you wind down or perhaps fall asleep. You can recover from anesthesia within an hour or so with a local anesthetic.
Ø IV anesthetic is administered through the vein in your arm. And you might be in a deep sleep throughout the procedure.
Your doctor might need to make a bone or gum incision to extract the teeth. In that case, the wounds will be stitched up to expedite their recovery. Within a few days, these sutures often fall out. They could also put sterile gauze in your mouth to tand control bleeding post extraction.
Post -Surgery Care
The next day, you will probably be able to resume your regular activities. Here is what you can do to expedite recovery and alleviate pain:
Ø If your jaw is painful or swollen, place a cool compress against it from time to time.
Ø Don’t spit excessively to avoid disturbing the blood clot and preventing the region from bleeding.
Ø While avoiding sodas, hot drinks and alcohol for at least 48 hours, drink plenty of water.
Ø Most likely, it will take a week or more before you can open your mouth completely. Eat only soft meals that will not irritate the region.
Post-Surgery Complications
While extracting the lower teeth, the surgeon occasionally triggers minimal nerve damage. Your tongue, chin, or lips might develop a persistent numbness. The procedure might harm your sinus and the breathing spaces under your eyes if done on your upper teeth. A painful disease known as dry socket might develop if your blood clot dissolves too quickly, leaving your bones and nerves exposed.
You must visit your dentist for a follow-up if you experience any discomfort post-surgery.
Root Tip | Apical Resection
Dental roots would always differ from person to person. For instance, you may find some people with lateral root canals and delta spaces. These little nooks and crannies are some of the most difficult-to-reach spaces in your mouth. That is why bacteria can quickly reproduce in these hard-to-reach corners.
The best way would be to fill in the gaps and create artificial blockage in the area to stop the bacteria from creating a base and spreading. However, conventional methods are unsuitable for doing this and end up allowing infection at the root tips. Hence, such a case calls for a solution that separates and removes the root tip region. As there is no area left for bacteria to grow, this minimizes the risk of infection. Root tip resection usually involves bone removal, cutting the root tip and closing it up.
Dental Cyst Operation
Dental cysts are the pathogenic tissues that appear inside your mouth. They can appear at any part of the jaw but are usually formed at the root tip of the teeth. However, they look like sacs wherever they form. Hence, before the treatment procedure, the dental practitioner would mandate DVT imaging, a 3D imaging technique to determine the exact borders of the cysts and allows for better and more accurate preliminary diagnosis using radiology.
However, it is essential to note that treatment procedures may vary depending on where the cyst is located. If a dental cyst has formed elsewhere, the first step would be to conduct a radiological exam and 3D imaging. The diagnosis step is more critical for analyzing the pathological risk than understanding the difficulty level of the surgery.